It has been a very full week. It has given me hope that things can turn back around. Last week, we had decided to give my body a break from chemo until after the trip. Late Monday, the cancer clinic called and said my 5th line of treatment, Havalen, had been approved and we were scheduled to start Tuesday. This news hit me with a lot of mixed feelings. I was worried about side effects ruining my trip, but the nurse assured me that this chemo is not known to have too many difficult side effects. The other fear, as always for cancer patients, is that too much time off treatment allows the cancer to run wild, so delays are scary. They agreed that if I did an infusion this week to see how it goes, I would be allowed to skip next week if I was worried about side effects during the trip. That sounded fair enough, so I agreed to get started.
Tuesday, I went in prepared to start. My medport had other ideas, though, and was not working properly. There was a lot of waiting. When all else fails, they inject a clot-buster and try to draw blood again every half hour. Three hours later, as we were about to give up, the port finally cooperated enough to draw blood for labs. At this point in the day, it was too late to do the chemo push, so I was rescheduled to come back and get some IV vitamins in addition to the chemo. While I was there, I also asked for an abdominal ultrasound, because my PleurX catheter suddenly stopped draining, though it was obvious that the fluid was still building up. Sure enough, the ultrasound showed a moderate amount of fluid, so an order was put in for a line-study on the medport to find out why it was so temperamental and a paracentesis and possible replacement of the PleurX catheter.
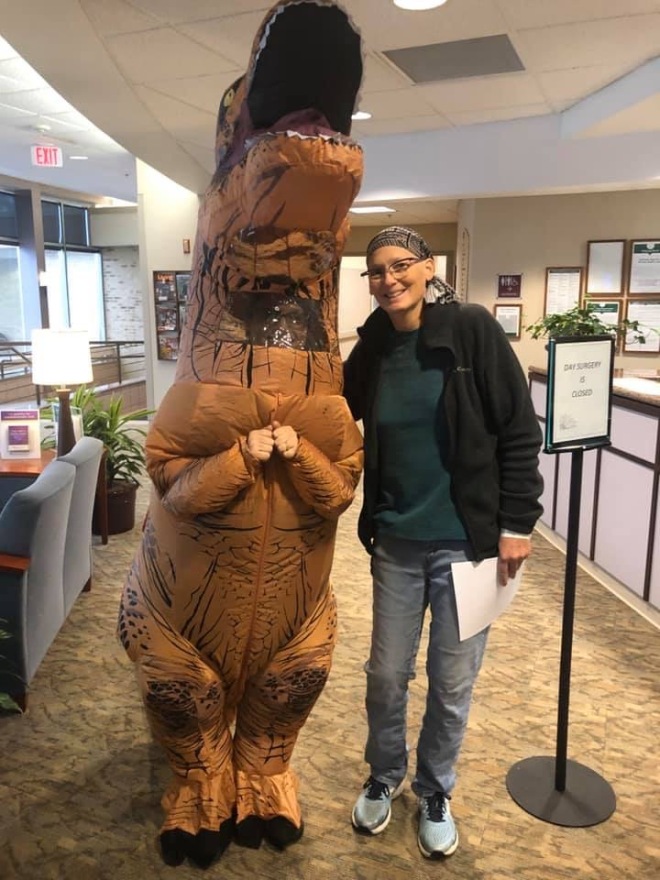
Wednesday, I was back at the clinic bright and early, since I had to be at the consultation at Froedert at noon. Everything flowed beautifully this time. What a difference a day makes! The port worked without any hassle, and the infusion was started promptly. Right as I was asking the nurse about the orders for the port and PleurX, Interventional Radiology called and scheduled the procedures for Friday at 6:00am. We finished everything without incident and I had time to get to Froedert early enough to have a nice tea date with my SIL!
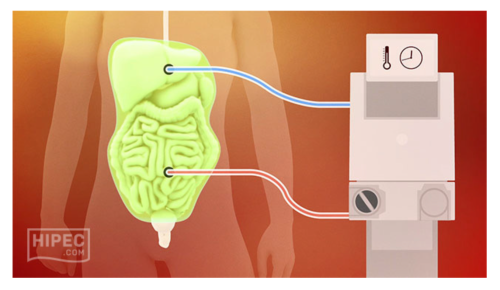
Then, at noon, Andy met me and it was time for the consultation about the HIPEC surgery (see my previous blog for more on HIPEC) I’ve been so hopeful about. It went really well. I liked the Doctor. He explained everything very clearly and answered all of our questions. His concern now is that I’ve lost too much weight and may be too weak for surgery. He arranged for his nutritionist to come in after we were done talking so she could help me gain weight and get ready to handle the surgery.
With peritoneal mets, the cancer causes inflammation and fluid builds up in the peritoneum (the lining around the digestive tract). I’ve been dealing with that for many months. My tumors are located in the omentum, which is another protective lining that drapes over the stomach, colon and intestines. The way the mets progress is the tumors grow out of the omentum and into the organs. So, the Doctor explained that we wouldn’t know if the surgery was a go until the day of surgery. He would start with an exploratory laparoscopy to see the extent of the tumors and the condition of the omentum. If the omentum is still free-floating and separate from the organs, he can proceed to remove the tumors or even remove the entire omentum. That may involve opening me up, if the omentum has become concrete-like with tumors. If the tumors have grown into the organs and everything is “stuck” together, then he will be unable to do the procedure, and that will be the end of that.
I am scheduled to see him again in two weeks to do another CT scan and at that point we can schedule the surgery. I’m encouraged that I’ve cleared the first hurdle and am being considered a candidate for surgery. In the meantime, Andy gave them our insurance liaison’s contact information and the requirements she set out so they could approve the surgery for payment. Hopefully, that will be very helpful in getting everything approved.
The meeting with the nutritionist was one of the most productive meetings I’ve had! I learned so much. She gave me exceptionally helpful advice, including lists of snacks and meals that my digestive system can handle, and what to avoid. She advised me to eat something small every two hours, and she gave me a whole bag full of different high calorie shakes and nutrition bars and powders. I’m on a mission now to gain the weight back so I can have the surgery.
It’s a lot to take in. A lot to think about. Overall, it was a good week and I’m very hopeful that HIPEC can give me some relief from the effects of the cancer in my abdomen. Now, tomorrow I need to be prepared for a 6am surgery to fix the medport and the pleurX catheter. One step at a time. Being able to drain the fluid will go a long way to help me stay comfortable and it will increase my appetite, too. And then my homework is to go to Disney and get fit and try to fatten up a bit! And have fun with my family. All this will be waiting for me when I get home.


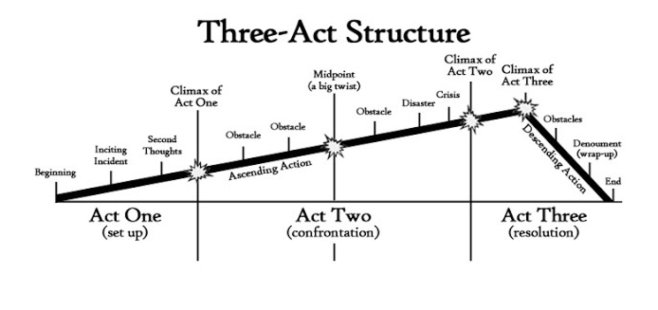 When I wrote the last two blog posts my husband, Andy, kept telling me to write the third act to give hope to my readers. He is a writer and a theater buff, so he frequently talks about Three Act Structure. Really, he actually does… He says that everything always goes terribly wrong in the second act and that things resolve in the third act. He wants me to hurry up and write part three since the last two posts felt rather tragic and hopeless. I know we’ll get to the third act but, unfortunately, we have a few more obstacles to deal with in act two.
When I wrote the last two blog posts my husband, Andy, kept telling me to write the third act to give hope to my readers. He is a writer and a theater buff, so he frequently talks about Three Act Structure. Really, he actually does… He says that everything always goes terribly wrong in the second act and that things resolve in the third act. He wants me to hurry up and write part three since the last two posts felt rather tragic and hopeless. I know we’ll get to the third act but, unfortunately, we have a few more obstacles to deal with in act two.