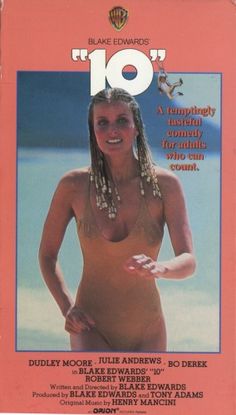
Okay, the image of Bo Derek from the movie “10” has nothing to do with this blog post, but it came to mind when I wrote the title, and I thought it was humorous, so there she is…. On a more serious note, this post is about re-defining what my own “perfect 10” means after the last few years and, of course, after turning 50 (loud and proud!!!) I’m also rounding out my surgery count at a perfect 10.
I didn’t learn from my last blog post, because the first big thing I’m tackling on my “50 after 50 List”, exactly one week after my 50th birthday, is surgery number TEN – check. I’m aiming for a perfect 10. I’m quietly hoping that the nice, round number 10 will symbolize my last time under the knife, but I’m not holding my breath. If I’ve learned anything in my 50 years on planet earth, it’s that life does not fit into the neat little, predictable boxes we may envision for ourselves. I won’t waste my energy worrying about how many more surgeries I might have in my future. I’m going to focus all my energy on the present surgery.
January 26th will be surgery number ten. Guess what? It’s not the knee surgery you might have anticipated due to my recent accident, rather I’m back at it with the plastic surgeon in Chicago. A lot of people have asked me what this surgery involves. They say, “I thought you did that surgery last year.” It’s complicated, so let me try my best to clarify why I am traveling to Chicago once again for surgery – Andy and I are calling it a “destination surgery”. I know, it is exotic. We did the same thing last January, and Andy still doesn’t let me count it as a honeymoon.
I’ve had a year to recover from Phase One. I’m not gonna lie to you- I’m still not fully recovered. It was one of the tougher ones, and I’m a bit of a connoisseur. My recovery goal was to build my strength back up and get as close to “normal” as possible before Phase Two. My method for recovery was volunteering with Team Phoenix, and completing the Tri-Ing for Children’s Triathlon, and (almost) the J-Hawk Late Bird. As you know, I never made it to the Late Bird, thanks to my rendezvous with a Jeep.
By September, I was feeling strong and setting my sights on a late fall surgery, leaving time to come back in 2018 for the Madison IronMan. My surgeon in Chicago knew that I wanted to have surgery after the September 24th triathlon. Ironically, they called me just after my accident with an opening – October 13th…. With the Honor Flight on October 14th, there was no way I was going to take that date. Anyway, I needed more time to let my knee and bruising heal before going through more trauma (I’m guessing the fat grafting won’t be coming from my thigh with this bruising). It would have to wait. Next available date would be January 26th. I’m so good at hitting “new year, new deductible….

ouch!
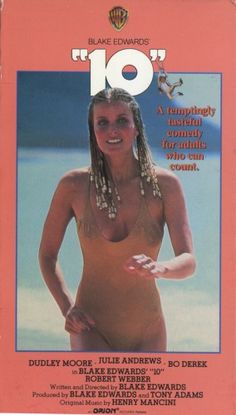
Now, I am more than ready to get on with it. So, back to what this surgery is all about. This is Phase Two DIEP Flap breast reconstruction. If you look back at my post called “Ninth One’s a Doozy”, you will get a little more background on Phase One of this process, which I completed a year ago. In a nutshell, Phase One is the major “relocating” of tissue from my abdomen to my chest to reconstruct a breast post-mastectomy. That surgery included a Lymph Node Transfer in an effort to control my Lymphedema. This is the reason I am traveling to Chicago for surgery. Very few surgeons do this surgery.
Phase Two involves sculpting and tweaking to try to make my DIEP flap match my other implant side. I’m not going for a perfect 10. I am hoping to be done with the awkward 4.5 I’ve been since the double mastectomy, though. People “in the know” will recognize terms such as “Ken Doll”, “Dog Ears”, and “Fat Necrosis”. These are some of the unsightly, and painful issues that can be fixed in phase two. For more on that, go ask Dr Google (actually, don’t! I just did a google images search, and it ain’t pretty). The fat necrosis is the worst. It causes me pain every day. The other stuff is just embarrassing in a locker room.
Phase 2 will also involve a lymphovenous bypass in my arm as a further attempt to alleviate the swelling caused by my lymphedema. It involves micro surgery in my arm to re-route the lymph vessels into the veins, so that the veins can carry the excess lymph fluid out of my arm. Sounds pretty cool, in theory. I’ll let you know how it feels next week.

I’ve said it before and I’ll say it again, “wish me luck….no….wish my surgeon luck-I’ll be sleeping.”

 Before the hospital gown hit the bottom of the soiled linens hamper, the ink was dry on the letter from the insurance company. The ink was dry on lines stating “we have determined that the service is not medically necessary,” and “We did not receive any other medical information to make a decision about your admission. We do not have your test results. We do not have reports about your care. You were admitted 01/06/2017. Your admission is not covered.”
Before the hospital gown hit the bottom of the soiled linens hamper, the ink was dry on the letter from the insurance company. The ink was dry on lines stating “we have determined that the service is not medically necessary,” and “We did not receive any other medical information to make a decision about your admission. We do not have your test results. We do not have reports about your care. You were admitted 01/06/2017. Your admission is not covered.”






 I have always loved travel. I dream of full time travel with my husband. I dream of “road-schooling” my children, broadening all of our horizons, and seeing the world. I have done a fair amount of travel, and I want to share this passion with my kids. My husband,
I have always loved travel. I dream of full time travel with my husband. I dream of “road-schooling” my children, broadening all of our horizons, and seeing the world. I have done a fair amount of travel, and I want to share this passion with my kids. My husband,