Rewind one year. Last fall, I started feeling like I had a bowling ball in my gut. My appetite was poor and I was generally uncomfortable. An ultrasound back in January of 2019 showed ascites (fluid in the peritoneal space or the sac around the digestive tract), but it was inaccessible to drain by paracentesis. So, I waited and hoped for relief from treatment. Last spring, the problem kept getting worse. I was starting to look pregnant and suffered heartburn, pain, digestive issues, and a major loss of appetite. Scans showed some fluid, but nothing too concerning. In June, I managed to have an amazing trip to Seattle with good friends. In July, I took a family vacation to the west coast, but I was not well. I pushed through. The memories with my family will always come ahead of anything else.
At the end of July, I was on another camping trip with my family and friends for the Team Phoenix annual triathlon. I was miserable. I had to tell everyone to go ahead without me while I let the pain pills kick in. If this triathlon hadn’t been such an important event in my life, I would have gone to the ER right then. But the pain pills helped and I made it through the triathlon to cheered this year’s athletes to the finish line. Somehow, I packed up camp (with a lot of help) and headed home. The next day, I was packed and ready to go to the ER. CT scans clearly showed a lot of fluid had accumulated, confirming what I knew all along. The ER doc gave me the choice to leave and arrange a paracentesis with my oncologist, or to be admitted and have the procedure the next day. I couldn’t stand it anymore, so I was admitted. I made the right choice, because by bedtime, I couldn’t eat, I was throwing up, and I couldn’t get comfortable sitting, laying down, standing or anything.
What is a paracentesis? Well, it starts with a “Little pinch and a burn,” something every doctor says (I swear there must be a course in medical school entitled “a little pinch and a burn…) as they push the needle gradually deeper into the abdomen with a numbing agent. It hurts. After the needle is withdrawn, a catheter remains in place and the tube is connected to a vacuum sealed bottle which draws the fluid out. They were able to draw 4.2 Liters of fluid, and the relief was immediate. It did not last, though. Less than two weeks later, I had to have another 3.8 Liters removed. The doctor told me that each liter of fluid weighs 2.3 pounds. And, interestingly, it is spot on. I’ve weighed myself before and after each procedure and the weight loss confirmed the amounts.
The fluid build up signals cancer’s progression. It was time to switch to a new line of treatment. This time we decided to go with a more aggressive IV chemo, and I was scheduled to have a MedPort inserted to make the chemo infusions easier. At the same time, I could feel the fluid building up again, so I called my oncologist to ask if I could have another paracentesis while I was in surgery for the Port. It had been less than a week since my last paracentesis and the fluid was accumulating faster that any of us anticipated. My doctor decided to put in an order for me to have a PleurX Catheter (a tube that remains in place to make draining easier) placed into my abdomen during Thursday’s surgery. My understanding was that they could drain it during surgery, and then I would be able to better control when to drain it at home, instead of waiting for appointment after the symptoms have gotten so bad.
The PleurX turned out to be a good idea, and I was draining 2 Liters every other day for several weeks while the chemo took time to build up in my system. Then a welcome thing happened. Around the 3rd week into chemo, I started getting less fluid when I drained, until there was barely a trickle. My symptoms resolved as my stomach flattened back out. The chemo was working! After nearly a month without any sign of fluid accumulation, it was determined that the PleurX could come out.
Now they say hindsight is 20/20 and it’s never worth second guessing past decisions, but it soon became clear that we shouldn’t have been so quick to take the catheter out. My relief from symptoms only lasted a couple of weeks and then the fluid started to build with a vengeance. I knew this was bad news. My oncologist does not have a good poker face, and as soon as I saw her I knew it was bad. The cancer had stopped responding to the chemo. She ordered an ultrasound and confirmed that I needed a paracentesis. This was a difficult blow for me. I had just started feeling good for the first time in months. And I had grown accustom to the ease (and painlessness) of draining with the PleurX. I was devastated when they told me to schedule the procedure immediately.
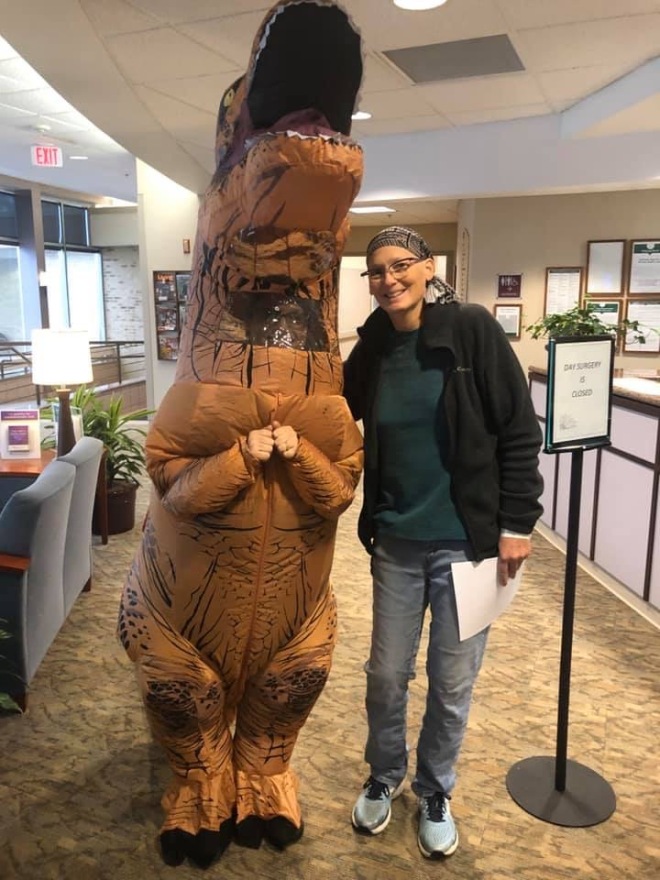
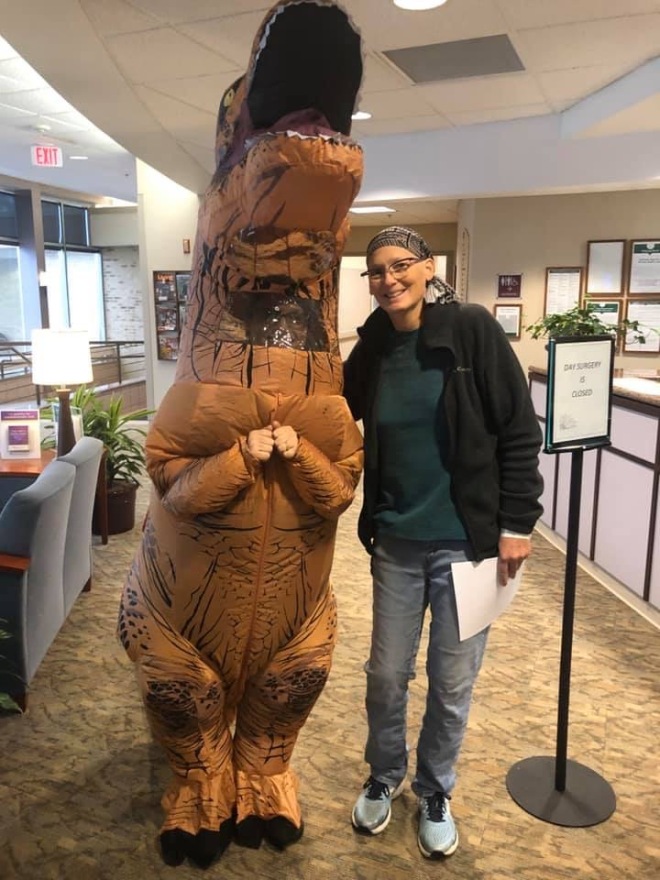
I was scheduled for the procedure on Halloween. I was dreading it and spent the day prior in tears, fearing the painful procedure. Andy did his best to comfort me, but he too knew the implications of having the fluid come back so fast. The mood was dark. The day started to turn around for me when I got to the hospital. The mood was festive for Halloween and the talk was all about the unusual Halloween snow storm, trick or treating and candy. By the time I got into the procedure room, I was feeling less anxious, almost relaxed. The nurses were amazing and we had great conversations about travel and life and kicking cancer’s ass! After the “little pinch and the burn”, the procedure went smoothly and I felt much better. After it was done, they asked if I wanted a dinosaur escort to back to the waiting room and my loving husband. I immediately jumped on that and said, “heck yeah, who wouldn’t want a dinosaur escort?!” The nurse struggled and squirmed back into her T-Rex costume and we made our way through the halls. It was the best walk down a hospital corridor I’ve ever had. People smiled. Heads turned. High fives were given (which is funnier than you would imagine with short little T-Rex arms). It’s amazing how the little things can do so much to turn a mood around. I ended up having a good Halloween after all.
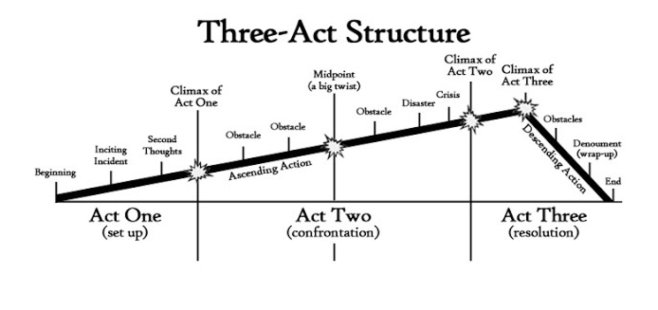 When I wrote the last two blog posts my husband, Andy, kept telling me to write the third act to give hope to my readers. He is a writer and a theater buff, so he frequently talks about Three Act Structure. Really, he actually does… He says that everything always goes terribly wrong in the second act and that things resolve in the third act. He wants me to hurry up and write part three since the last two posts felt rather tragic and hopeless. I know we’ll get to the third act but, unfortunately, we have a few more obstacles to deal with in act two.
When I wrote the last two blog posts my husband, Andy, kept telling me to write the third act to give hope to my readers. He is a writer and a theater buff, so he frequently talks about Three Act Structure. Really, he actually does… He says that everything always goes terribly wrong in the second act and that things resolve in the third act. He wants me to hurry up and write part three since the last two posts felt rather tragic and hopeless. I know we’ll get to the third act but, unfortunately, we have a few more obstacles to deal with in act two.